Acute Respiratory Illnesses and exercise
This is an excerpt from Medical Conditions in the Physically Active 4th Edition With HKPropel Access by Katie Walsh Flanagan & Micki M. Cuppett.
Acute Respiratory Illnesses
Several acute respiratory illnesses are mainly caused by viral infection, and most present with similar symptoms. Common acute respiratory illnesses include influenza (types A and B), severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and resultant coronavirus disease 2019 (COVID-19), and respiratory syncytial virus (RSV). In this chapter, these illnesses are grouped together because of their similar signs and symptoms. Often, the specific acute respiratory illness cannot be confirmed via clinical examination and antigen tests are necessary to ascertain its exact nature.
Influenza, generally known as the flu, is a common viral infection. Outbreaks of influenza in the United States usually occur during the fall and winter months. Since 2010, an estimated 12,000 to 61,000 people have died from influenza annually in the United States. Various influenza strains (mainly types A and B) can cause epidemic outbreaks and lead to thousands of hospitalizations each year. In recent years, however, other strains have emerged, including avian and swine influenza (see chapter 14).
SARS-CoV-2, COVID-19, and RSV also have several influenza-like symptoms and usually cannot be differentiated from influenza type A or B without rapid molecular assay testing. There is some evidence that influenza A may lead to increased susceptibility to SARS-CoV-2 and more severe disease. RSV can infect all age groups but is most dangerous in infants and older adults; its symptoms are similar to rhinovirus (the common cold) but can include fever and wheezing. Chapter 14 further describes the spread and effects of SARS-CoV-2 and other types of influenza.
This chapter focuses mainly on signs and symptoms of acute respiratory illnesses and patient referral. People most susceptible to severe complications are considered high risk and include older adults, individuals who live in close quarters (e.g., students), and those with compromised immune systems, diabetes, or chronic heart, lung, or kidney disease. Influenza is transmitted from person to person via contagious droplets that spread when an infected person sneezes or coughs (figure 6.10).

Signs and Symptoms
Milder forms of influenza can be confused with other viral URIs, such as the common cold; however, patients with influenza are generally sicker. Onset of influenza symptoms is rapid and can include high fever, headache, muscle ache, cough, chest pain, shortness of breath, fatigue, loss of appetite, nasal congestion, and sore throat. One clue that aids diagnosis is the reported contact with others diagnosed with influenza. Complications may include secondary bacterial infections, such as sinusitis or pneumonia. Influenza also can cause pneumonia and encephalitis (infection of the brain).
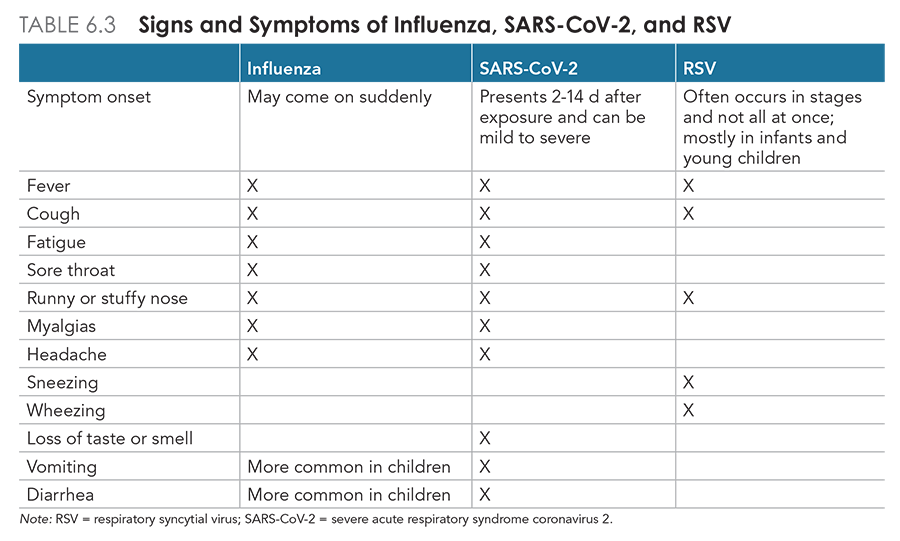
Influenza must be differentiated from SARS-CoV-2, RSV, sinusitis, bronchitis, pneumonia, and other URIs. Compared with influenza type A, symptoms of SARS-CoV-2 infection may take longer to develop. Young adults with RSV may experience mild symptoms similar to the common cold, although the virus is more common in infants and young children and their symptoms are more severe. Fever is a hallmark among patients with influenza, SARS-CoV-2, and RSV, whereas those with sinusitis are typically afebrile. COVID-19 spreads more easily than influenza, can cause more severe illness in vulnerable populations, and may present with cardiac or other symptoms (see chapter 7). Although COVID-19 has some differences in clinical features compared with influenza and RSV, their presentation and comorbidities overlap significantly (table 6.3).
Referral and Diagnostic Tests
Diagnosis is usually made on clinical grounds, but influenza and COVID-19 cannot be differentiated clinically. Rapid testing for SARS-CoV-2 infection is now common because of the COVID-19 pandemic. To differentiate between SARS-CoV-2, influenza, and RSV infection, the athletic trainer should use a specific rapid test or a combination polymerase chain reaction (PCR) collection kit to immediately test symptomatic patients and individuals in close contact with someone diagnosed with influenza or SARS-CoV-2. Rapid tests provide quick results, whereas combination PCR tests must be sent to a laboratory for analysis. Additional laboratory tests, including a complete blood count (CBC), can be used to delineate viral versus bacterial infection, and blood and sputum cultures obtained in severe illness can isolate pathogens and determine the presence of bacteremia. Chest radiographs should be ordered if pneumonia is suspected on clinical examination.
Treatment and Return to Participation
For generally healthy individuals, treatment for influenza, COVID-19, and RSV is mostly supportive and includes bed rest, analgesics for muscle aches and pains, and increased fluid intake for mild illness. The patient should be sent home to rest and should avoid contact with other individuals to limit disease spread. If influenza is diagnosed within 48 h of symptom onset, several antiviral medications may shorten the symptom duration by approximately 1 d in high-risk groups. These medications include oseltamivir (Tamiflu), zanamivir (Relenza), peramivir (Rapivab), and baloxavir marboxil (Xofluza). The recommended antivirals change yearly, depending on the most common strain of influenza within the population. In most individuals who are otherwise healthy, influenza fully resolves within 7 to 10 d.
Some antiviral agents, such as nirmatrelvir (Paxlovid), can be administered to patients with SARS-CoV-2 infection. However, health care providers should consult the latest U.S. Centers for Disease Control and Prevention (CDC) treatment recommendations, because they are updated frequently. COVID-19 may take longer to fully resolve; however, the patient may return to low-level activities when they feel able and are no longer contagious. Among individuals in high-risk groups, both influenza and COVID-19 may be severe and can lead to complications, including pneumonia. Patients recovering from influenza are usually fit to return to activity in 1 to 2 wk, but they must be afebrile and have no respiratory compromise at rest, such as shortness of breath or pleuritic chest pain.
Prevention is the best approach in the management of influenza. Depending on the supply of vaccine, the athletic trainer should encourage all patients to be immunized yearly against common strains of influenza. Immunization typically begins in late October and early November. Individuals at high risk are generally immunized first. The influenza vaccine has a variable success rate from season to season, generally ranging from 60% to 70% in people with normal immune systems. See chapter 14 for more information on recommended vaccination schedules. Vaccinations are available for intramuscular or intradermal injection or for intranasal administration, and the nasal spray form can be given to children as young as 6 mo.26 The main challenge for the athletic trainer is to reduce exposure among patients and athletes, especially during travel. Use of face masks to reduce virus transmission is now common in medical facilities and other close quarters. Other means of prevention, especially for the athletic population, include handwashing and not sharing drinking receptacles or bench towels.
SHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW


